For patients recovering from opioid use disorder there are three drugs currently available for treatment: methadone, buprenorphine, and naltrexone. All three of these drugs attach to opioid receptors in the brain preventing heroin or prescription opioid drugs from binding and helping to reduce craving in patients. But given the ongoing opioid crisis and the high rate of relapse there is an urgent need for more options.
“Treatment is not one size fits all—what may work for one patient may not work for another,” said Amanda L. Persons, Ph.D., Associate Professor and Director of the Facility for Rodent Models of Human Brain Disease in the Center for Compulsive Behavior and Addiction at Rush University Medical Center in Chicago. Dr. Persons was one of two recipients of opioid research grants from BRF in 2018.
Dr. Persons and her collaborator, Dr. Celeste Napier, looked for alternate targets in the brain that may help reduce opioid craving during recovery. The team’s previous work studying relapse to methamphetamine use in rats led them in a promising direction. They discovered that targeting a serotonin receptor called 5-HT2CR using the antidepressant mirtazapine reduces relapse-like behavior in rats trained to self-administer methamphetamine.
“It’s kind of like the 5-HT2CR receptor is always turned on [in these animals] and mirtazapine is able to shut it off,” she explained. The finding was particularly exciting because mirtazapine has already been shown to be safe, well-tolerated, and effective for depression treatment in humans. “Repurposing an existing drug shaves a lot of time off the process of getting medications into the clinic to test them in humans,” Dr. Persons explained. To begin to test whether mirtazapine might also help prevent relapse in opioid use disorder, Dr. Persons and her team tested using mirtazapine in rodents conditioned to associate a specific environment with morphine. They found that rodents treated with mirtazapine were less likely to spend time in the environment where they received morphine—the rats were spending less time seeking the drug. Such environmental cues have been shown to trigger drug craving and relapse in humans as well.
Dr. Persons’ findings are particularly exciting because the drug she is investigating to treat opioid relapse is already approved for use in humans.
“Relapse to drug taking is not so much about the drug itself anymore,” Persons explained. Instead, it is often about the associations a person has developed between the feeling they got taking a drug and the places, people, and paraphernalia they associate with it. “Maybe through cognitive behavioral therapy and pharmacological therapy, we can temper down those cravings and make them manageable for people,” she said.
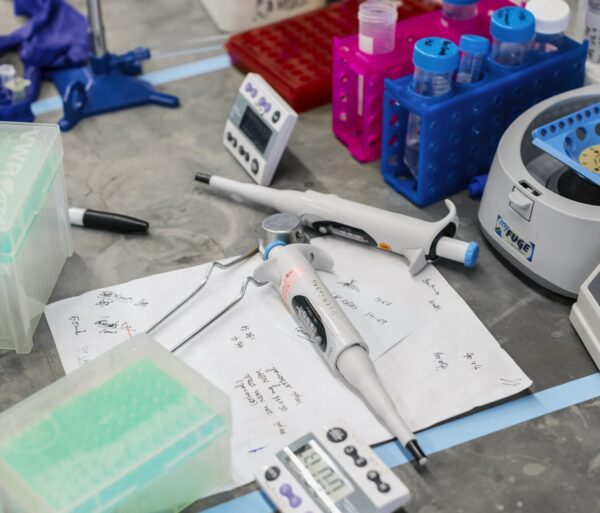
The grant from BRF allowed Persons and her team to take the next step by testing whether mirtazapine can reduce relapse-like behavior in rats trained to self administer heroin, a gold-standard model for addiction research. They also documented the changes that occur in the 5-HT2CR receptors in response to heroin use, relapse, and mirtazapine treatment.
Dr. Persons planned to publish her results. She hopes that her work will not only lead to more treatment options, but also help destigmatize relapse—a goal BRF shares. Relapse is common in many other chronic conditions as well, Dr. Persons explained, but patients who experience a relapse to substance abuse often face judgment.
“Addiction is a brain disease,” Dr. Persons said. “It causes biochemical and structural changes in the brain.”
By identifying and helping to fund research that reveals those changes and finds ways to reverse them, BRF hopes to help stem the ongoing epidemic and provide relief for the individuals and families affected by it.